Credit: Original article published here.A new study conducted by researchers at the Johns Hopkins Bloomberg School of Public Health found an association between common infections and poor cognitive performance. The research was published in Alzheimer’s & Dementia. Senior author and professor at the Bloomberg School’s Department of Mental Health, Adam Spira, PhD, stated: “The idea that common infections could contribute to cognitive decline and perhaps Alzheimer’s disease risk was once on the fringe and remains controversial, but due to findings like the ones from this study, it’s starting to get more mainstream attention.” Dr. Spira and his research team analyzed the antibody levels of five common pathogens which included: herpes simplex virus, cytomegalovirus (CMV), Epstein-Barr virus, varicella zoster virus, and Toxoplasma gondii. Mini-Mental State Examination (MMSE) and delayed verbal recall performance were evaluated in 575 adults aged 41 to 97 years who donated blood for testing as part of the Epidemiologic Catchment Area Study. Researchers employed multivariable-adjusted zero-inflated Poisson regression models to analyze the data. The results showed that having positive antibody tests for CMV (P =0.011) and herpes simplex virus (P =0.018) were individually linked to poorer performance on the MMSE. Additionally, the study found that having a greater
Credit: Original article published here.New data from a study funded by the National Institutes of Health reported that children with multisystem inflammatory syndrome (MIS-C) have a distinct biomarker that is not present in other children with COVID-19. MIS-C is a rare condition linked with SARS-CoV-2 infection that is marked by external and internal inflammation. The study, which was published in Cell Reports Medicine, was conducted by Charles Y. Chiu, MD, of the University of California San Francisco, and colleagues from other institutions. The investigators used next-generation sequencing to analyze 416 blood samples from 141 children diagnosed with MIS-C and 70 children with acute COVID-19. Additionally, 26 controls were included in the study. After analysis with plasma cfRNA profiling, the researchers identified signatures associated with cell injury and cell death that distinguished between patients with MIS-C and acute COVID-19. wbRNA analysis showed overlap in pro-inflammatory pathways between samples with MIS-C and COVID-19, as well as pathways specific to the respective disease states. Based on plasma cfDNA methylation profiling, patietns with MIS-C had increased cfDNA and solid organ involvement compared with patients with COVID-19 and controls. Upon comparative analysis, the investigators found that cfRNA and wbRNA samples yielded separate, but complementary signatures
Credit: Original article published here.In a recent study, researchers evaluated treatment adherence in patients with asthma or chronic obstructive pulmonary disease (COPD) based on age and either once-daily or twice-daily dosing of medication. They generally sought to determine if prescribing once-daily dosing improved the suboptimal treatment adherence seen in this population. The study’s lead author, Heather De Keyser, MD, MSCS, reported that patients with asthma and COPD with once-daily medications had significantly improve daily treatment adherence compared with patients prescribed twice-daily medications. Researchers also found patients with COPD showed higher adherence than patients with asthma, which they noted may be due to an older cohort age. Findings from the study were presented in The Journal of Allergy and Clinical Immunology: In Practice. Treatment Adherence Improved With Once-Daily Medication The study assessed data from electronic medication monitors on date and time of inhaler actuations over 90 days among patients from the Propeller Health platform. Researchers compared adherence between once- and twice-daily schedules using retrospective regression models adjusted for age. According to the report, patients with once-daily schedules had a median daily adherence of 63.3% (interquartile range [IQR], 31.1-86.7) for asthma and 83.3% (IQR, 57.2-95.6) COPD, which was significantly higher than patients with
Credit: Original article published here.In this episode of Healthcare Unfiltered: Dr. Chadi Nabhan hosts a duo of Canadiens to discuss quality of life and patient-reported outcomes in clinical trials: Christopher Booth, MD, and Michael Brundage, MSc, FRCPC, MD, both of Queen’s University. They begin by pontificating on whether quality of life is a “must” endpoint in designing interventional clinical trials today, the timeline of how “PROs” came to be a term and an important component of clinical trials, and much more.
Credit: Original article published here.Researchers of a study, published in Radiotherapy and Oncology, evaluated the effects of post-mastectomy radiation therapy in patients with HER-2 positive breast cancer based on pathological response to previous primary systemic therapy. The analyses used pooled data from the TRYPHAENA and NeoSphere randomized phase 2 trials. According to the study’s lead author, Omran Saifi, patients who achieved a complete nodal pathological response (ypN0) after primary systemic therapy had “excellent locoregional-control” that supported deescalation of post-mastectomy radiation therapy. Conversely, patients with ypN2-3 disease showed significant benefits with radiation therapy. Post-Mastectomy Radiotherapy Effect Per Nodal Status The analyses included 312 pooled patients with node-positive disease who were treated with HER-2-targeted primary systemic therapies, followed by mastectomy with or without subsequent radiation therapy. The primary end point was loco-regional recurrence-free survival (LRRFS). Researchers noted 172 (55%) patients achieved ypN0 response and 140 (45%) patients did not. Patients with ypN0 both with or without post-mastectomy radiation therapy had a 5-year LRRFS of 97% (P=.17). Patients with ypN1 disease (n=62) who received post-mastectomy radiation therapy (n=40) had a 5-year LRRFS of 89% compared with a LRRFS of 89% in those who did not receive radiation therapy (n=22; P=.60). In addition, authors found
Credit: Original article published here.A recent publication in JAMA Network Open explores two clinical questions related to antiphospholipid antibodies (aPL): (1) what is the prevalence of aPL positivity at a single time point, and (2) are aPL antibodies associated with future atherosclerotic cardiovascular disease (ASCVD) risk? [1]. Antiphospholipid syndrome (APS) is an acquired condition that is characterized by a thromboinflammatory state, with arterial or venous thrombotic events and/or obstetric complications, in the presence of persistently circulating aPL antibodies. Arterial thrombotic events in APS include stroke or myocardial infarction (MI). With a recent study suggesting autoantibodies can be present in up to 18-32% of individuals [2], the authors of this study postulated whether presence of these autoantibodies may put individuals at higher risk for ASCVD morbidity than is currently recognized. Previous studies have demonstrated aPL are acutely present in up to 17.4% of patients with cardiovascular events such as stroke and transient ischemic attack, and some incidental positive aPL can be present in 1-12% of otherwise healthy individuals. Thus, this study sought to determine association of aPL and future ASCVD events and investigate association of sex, race, and ethnicity with aPL prevalence [1]. Zuo et al performed this population-based cohort study
Credit: Original article published here.There are no solutions, only tradeoffs. In acute myocardial infarction, we have tradeoffs between coronary supply and myocardial demand. In terms of supply, we have made significant progress by reducing ischemic time but see a plateau of benefit at 90 minutes. In terms of demand, we currently utilize pharmacotherapy which may be too little too late, especially in patients with large infarct size who have progressed to cardiogenic shock and cannot tolerate these therapies. We see these trends in the outcomes data. While advances in restoring supply have led to high short-term survival rates, long-term outcomes remain challenging due to the incidence of heart failure which reaches nearly 75% at 5 years (1). In-hospital mortality for cardiogenic shock remains abysmal despite advances in reperfusion. Thus, it is paramount that we find therapies capable of limiting infarct size without compromising systemic perfusion. Mechanical unloading is one option that has been shown to reduce infarct size in preclinical studies since the 1980s. Translating the efficacy of preclinical studies to effectiveness in the real world, however, remains a work in progress. The initial roadblock was inadequate technology. In 2008, the FDA approved the Impella, a percutaneous transaxial flow pump,
Credit: Original article published here.The implantable cardioverter defibrillator (ICD) is frequently utilized in patients with heart failure for primary and secondary prevention and treatment of unstable arrhythmias. This device is a unique medical intervention that may improve survival for select patients but does not necessarily improve quality of life and may even lead to detrimental impacts. At the 2023 Houston Shock Symposium, Dr. Haider Warraich – director of the heart failure program at VA Boston Healthcare, assistant professor at Brigham and Women’s Hospital and prolific author highlighted the psychological stress that can impact ICD recipients and the physician role in addressing these stressors with our patients. Psychological stressors can present in many ways in ICD recipients; ranging from feeling phantom shocks to avoiding engagements due to fear of shock and persistent hyper-vigilance. Identified risk factors for increased psychosocial distress in ICD recipients include younger age less than 50 years old, female gender, low social support, premorbid psychiatric diagnosis, and greater than 5 appropriate or inappropriate defibrillations.1 Dr. Warraich challenged healthcare providers at the Houston Shock Symposium to consider the physician role in empowering patients to shift their mindset after an ICD shock from victimhood thinking with poor coping skills to
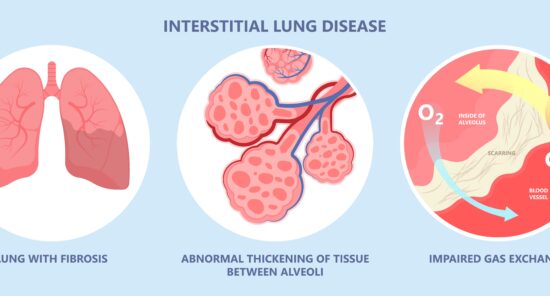
Credit: Original article published here.In a recent study, published in Rheumatology International, researchers sought to determine predictive variables for development of interstitial lung disease (ILD) among patients with rheumatoid arthritis (RA), a common complication associated with increased morbidity and mortality. After retrospective analysis, the study’s lead author, Gouri Mani Koduri, and colleagues developed a novel risk-stratification model for ILD in patients with RA based on 4 clinical variables: age, smoking history, anti-cyclic citrullinated peptide antibodies, and rheumatoid factor. The investigators reviewed data on 430 patients with RA that was collected across 20 centers between 2010 and 2020. Of the participants, 210 had ILD confirmed by high-resolution computed tomography (HRCT). 4 Variables Effectively Predict Interstitial Lung Disease In independent variable analysis, researchers identified past or present smoking, older age, and rheumatoid factor/anti-cyclic citrullinated peptide positivity as key significant variables associated with risk of developing ILD among patients with RA. Using multivariate logistic regression models, the study’s authors constructed a 0-9 point scoring system with a threshold at 5 points for differentiating patients as high-risk or low-risk. The report noted the model had an area under the receiver operating characteristic curve of 0.76 (95% CI, 0.71-0.82), as well as a sensitivity and
Credit: Original article published here.Researchers, led by R. Nisha Aurora, MD, MHS, cited glycemic variability is linked to increased cardiovascular disease risk among patients with type 2 diabetes, regardless of glycosylated hemoglobin (HbA1c) levels. Additionally, studies on positive airway pressure (PAP) therapy for obstructive sleep apnea (OSA) have produced inconsistent findings regarding its effects on HbA1c levels. Dr. Aurora and colleagues sought to determine if PAP therapy improved glycemic variability in patients with moderate-to-severe OSA and type 2 diabetes. Overall, they reported PAP therapy did not appear to improve glycemic control or variability in this patient population. The study was presented in Chest. PAP Therapy Did Not Improve Glycemic Measures The authors’ randomized controlled trial enrolled 184 patients with type 2 diabetes and OSA . Participants were randomized to lifestyle counseling with or without PAP therapy for 3 months. The primary end points were standard deviation of glucose levels, additional continuous glucose monitoring (CGM) values, and self-monitored blood glucose. According to the report, the cohort’s average use of PAP therapy was 5.4 ± 1.6 hours per night. Overall, researchers found no significant differences between the 2 groups for any primary or secondary CGM end points; however, exploratory analyses found some