Credit: Original article published here.New data from a study funded by the National Institutes of Health reported that children with multisystem inflammatory syndrome (MIS-C) have a distinct biomarker that is not present in other children with COVID-19. MIS-C is a rare condition linked with SARS-CoV-2 infection that is marked by external and internal inflammation. The study, which was published in Cell Reports Medicine, was conducted by Charles Y. Chiu, MD, of the University of California San Francisco, and colleagues from other institutions. The investigators used next-generation sequencing to analyze 416 blood samples from 141 children diagnosed with MIS-C and 70 children with acute COVID-19. Additionally, 26 controls were included in the study. After analysis with plasma cfRNA profiling, the researchers identified signatures associated with cell injury and cell death that distinguished between patients with MIS-C and acute COVID-19. wbRNA analysis showed overlap in pro-inflammatory pathways between samples with MIS-C and COVID-19, as well as pathways specific to the respective disease states. Based on plasma cfDNA methylation profiling, patietns with MIS-C had increased cfDNA and solid organ involvement compared with patients with COVID-19 and controls. Upon comparative analysis, the investigators found that cfRNA and wbRNA samples yielded separate, but complementary signatures
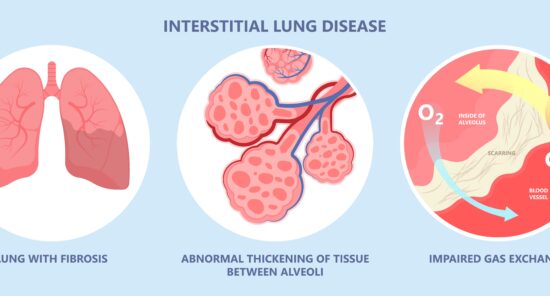
Credit: Original article published here.In a recent study, published in Rheumatology International, researchers sought to determine predictive variables for development of interstitial lung disease (ILD) among patients with rheumatoid arthritis (RA), a common complication associated with increased morbidity and mortality. After retrospective analysis, the study’s lead author, Gouri Mani Koduri, and colleagues developed a novel risk-stratification model for ILD in patients with RA based on 4 clinical variables: age, smoking history, anti-cyclic citrullinated peptide antibodies, and rheumatoid factor. The investigators reviewed data on 430 patients with RA that was collected across 20 centers between 2010 and 2020. Of the participants, 210 had ILD confirmed by high-resolution computed tomography (HRCT). 4 Variables Effectively Predict Interstitial Lung Disease In independent variable analysis, researchers identified past or present smoking, older age, and rheumatoid factor/anti-cyclic citrullinated peptide positivity as key significant variables associated with risk of developing ILD among patients with RA. Using multivariate logistic regression models, the study’s authors constructed a 0-9 point scoring system with a threshold at 5 points for differentiating patients as high-risk or low-risk. The report noted the model had an area under the receiver operating characteristic curve of 0.76 (95% CI, 0.71-0.82), as well as a sensitivity and
Credit: Original article published here.A randomized, placebo-controlled clinical trial did not find a significant clinical benefit of colchicine twice daily for pain relief in patients with osteoarthritis (OA) of the hand. Notably, treatment with colchicine was also associated with greater incidence of adverse events (AEs). These findings were published in Lancet Rheumatology. Colchicine is a medication used for the treatment of gout. It as anti-inflammatory properties, but there is limited evidence of its benefit for treatment of other conditions. This single-center study enrolled 100 patients with symptomatic hand OA and finger pain who were treated at an outpatient clinic in Denmark. Inclusion criteria was a pain rating of at least 40 mm out of 100 mm on the visual analog scale (VAS). The target hand was the hand with the most severe finger pain at baseline. The study was double-blinded, and patients were randomized to either 0.5 mg colchicine or placebo taken orally, twice daily for a period of 12 weeks. Patients were stratified according to sex, whether their age was ≥75 years, and whether their body mass index (BMI) was ≥30 kg/m2. The primary endpoint was changes in target hand pain at 12 weeks, assessed via VAS. The researchers
Credit: Original article published here.Different biological immunotherapies for the treatment of psoriasis are associated with variable delays in progression to inflammatory arthritis, according to a retrospective study in Lancet Rheumatology. In particular, inteurleukin (IL)-12/23 and IL-23 inhibitors demonstrated the greatest benefit in time to progression to inflammatory arthritis compared with other immunotherapies. Shikha Singla, MD, and colleagues used electronic health records data to identify adults in the US who were newly prescribed a biologic therapy for psoriasis. Treatments included in the study were: Tumor necrosis factor (TNF) inhibitor IL-17 inhibitor IL-23 inhibitor IL-12/23 inhibitor Patients were included in the study if they had at least two diagnostic codes for psoriasis (>30 days apart) and a newly prescribed biologic between Jan. 1, 2014, and June 1, 2022. In total, 15,501 patients with psoriasis met inclusion criteria. The mean age was 50.2 years and 54.2% of patients were women. White patients made up 72.1% of the cohort. The time to incident inflammatory arthritis was defined by the first occurrence of a diagnostic code for psoriatic arthritis or other inflammatory arthritis following treatment with immunotherapy. The time-dependent risk was calculated with weighted Cox proportional hazards regression—anti-TNF exposure was the reference, and the researchers
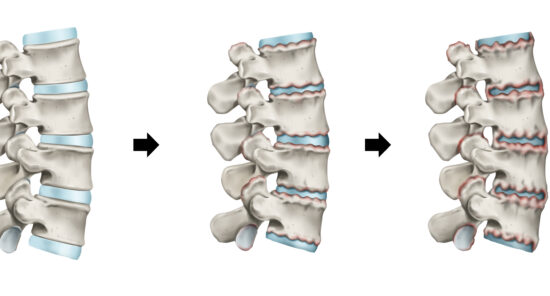
Credit: Original article published here.Telomere length shortening plays a role in the deterioration and death of various immune cells, leading to immune destabilization and ageing. Researchers, led by Donglei Wei, investigated if leukocyte telomere length (LTL) had a causal relationship with rheumatoid arthritis or ankylosing spondylitis (AS). Based on their Mendelian randomization (MR) study, the authors suggested longer LTL may be associated with increased risk of developing AS, and may play a role in spondyloarthritis progression. The study did not find evidence of a similar relationship between LTL and rheumatoid arthritis in analyses. The data were presented in Frontiers in Immunology. Telomere Length Linked to Spondyloarthritis The analysis encompassed 472174 LTL records from the UK Biobank genome-wide association study database, as well as 229640 patients with AS and 212472 with RA from the FinnGen database. Researchers used MR-Egger, inverse variance weighting, and weighted median methods to evaluate the causal effects of LTL on RA and AS. During forward MR analysis, investigators stated their inverse variance-weighted (IVW) and weighted median results suggested that longer LTL could be associated with increased risk of developing AS (IVW odds ratio, 1.55; 95% CI, 1.14-2.11; P=.006). In addition, MR-Egger regression models indicated there was no pleiotropy
Credit: Original article published here.Soumya Chakravarty, MD, PhD, FACP, FACR, Senior Director, Strategic Lead, Rheumatology Therapeutic Area at The Janssen Pharmaceutical Companies of Johnson & Johnson, discusses a post-hoc analysis of recent Phase 3 DISCOVER-2 study, which shows that early clinical improvement at eight weeks of joint and skin disease, enthesitis and dactylitis in adult patients with active psoriatic arthritis treated with TREMFYA® (guselkumab) were associated with meaningful improvements in health-related quality of life from year one through year two.
Credit: Original article published here.A new study published in JAMA Network Open suggests patients with granulomatosis with polyangiitis (GPA) are more likely to achieve remission if treated with rituximab for induction therapy compared to cyclophosphamide [1]. Previous clinical trials, such as the RAVE trial [2], demonstrated that rituximab was noninferior to cyclophosphamide for induction of remission in severe ANCA-associated analysis (AAV), with neither treatment having a specific advantage for GPA in adjusted analysis. However, post-hoc analysis showed higher remission rate for rituximab than cyclophosphamide in those with PR3 ANCA antibodies. Given some trial limitations with enrollment of patients with both GPA and microscopic polyangiitis, the authors of this study sought to perform an emulation target trial with observational data to compare rituximab vs cyclophosphamide efficacy at inducing remission in a large number of unselected patients with GPA. Puéchal et al performed a comparative effectiveness study using observational data from 32 French hospitals as part of the French Vasculitis Study Group Registry. Groups were determined according to treatments received. They included patients with newly diagnosed or relapsing GPA by ACR Classification Criteria and/or Chapel Hill Consensus Conference nomenclature with active disease who received at least 1 infusion of rituximab or cyclophosphamide
Credit: Original article published here.Decreasing body mass index (BMI) was independently associated to reduced progression of knee osteoarthritis (OA) on radiography, according to a study in Arthritis & Rheumatology. Being overweight (BMI 25 to <30 kg/m2) or obese (BMI ≥30.0 kg/m2) are known risk factors for the development and progression of knee OA, with nearly one-quarter of cases of new-onset knee pain or OA being attributed to excess weight. For this recent study, Zubeyir Salis and colleagues sought to use radiography to determine the association between BMI change and the progression of structural defects associated with knee OA. The team utilized baseline and 4 to 5 years of follow-up data from 3 independent cohort studies: the Osteoarthritis Initiative (OAI) study, the Multicenter Osteoarthritis Study (MOST), and the Cohort Hip and Cohort Knee (CHECK) study. They used logistic regression analyses to investigate the association between change in BMI from baseline through follow-up and the corresponding incidence and progression of knee OA during that timeframe. Exclusion criteria included knee replacement surgery prior to baseline. In total, 9,683 knees from 5,774 participants were included in an “incidence” cohort, and 6,075 knees from 3,988 participants were included in a “progression” cohort. The incidence cohort
Credit: Original article published here.In the phase 4 AWARE study, researchers compared golimumab and infliximab in patients with rheumatoid arthritis. After around 40% of AWARE participants reported no concurrent use of methotrexate, researchers conducted a post hoc analysis to evaluate golimumab with or without methotrexate for rheumatoid arthritis. Data were presented in BMC Rheumatology. The analysis’s lead author, Aaron Broadwell, reported that the efficacy of golimumab either with or without methotrexate was generally similar over 1 year, regardless of prior biologic treatment history. The report noted that real-world adverse event outcomes with golimumab were consistent with the previously described safety profile. Golimumab Performs Similarly With or Without Methotrexate The real-world, prospective, noninterventional AWARE study included 685 patients treated with golimumab, of which 420 (61%) were on concomitant methotrexate and 265 (39%) were not; authors added that 63% and 72% of the groups, respectively, discontinued the study. The efficacy of golimumab was evaluated based on mean change in Clinical Disease Activity Index (CDAI) at months 6 and 12 and safety was evaluated based on adverse events over 1 year of follow-up. Authors found patients in the golimumab with methotrexate group had a shorter mean disease duration compared with patients in the golimumab
Credit: Original article published here.Strong evidence suggests that patients with moderate to severe symptomatic osteoarthritis (OA) who have failed nonoperative treatment should proceed directly to surgical care, without additional nonoperative therapies, according to new guidelines from the American College of Rheumatology (ACR) and the American Association of Hip and Knee Surgeons (AAHKS). Elective Joint Replacement for Osteoarthritis The new guideline addresses the optimal timing of elective joint replacement for patients with symptomatic moderate to severe OA or osteonecrosis who are indicated for surgery after failure on nonoperative therapy. Along with information on surgical timing, the guideline also offers recommendations for when additional nonoperative treatment are appropriate for in this patient population. “For patients with symptomatic moderate to severe osteoarthritis or osteonecrosis of the hip or knee who have been indicated for total hip or total knee arthroplasty, the efficacy of additional nonoperative treatments, such as physical therapy, anti-inflammatories, and injections is unknown,” said Dr. Charles P. Hannon, MD, MBA, co-literature review leader of the guideline. “In addition, for patients with certain risk factors, such as obesity, which are linked to increased risk and poorer outcomes, the benefit of delaying surgery to modify these risk factors is not well established. For